What is AVM disease?
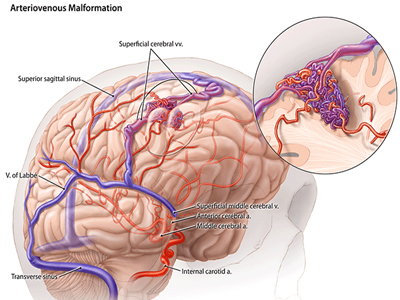
An arteriovenous malformation, or AVM for short, is a group of blood vessels that are abnormally interconnected with one another. AVMs can occur in different organs of the body, but brain AVMs are the most problematic. Another term for AVM is "arteriovenous fistula".
What are the symptoms of disease?
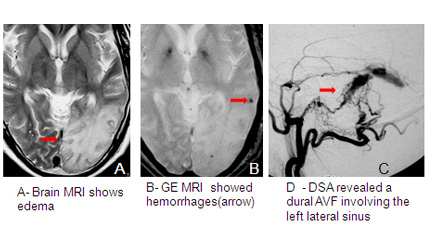
About half of the patients find out they have an AVM only after they suffer a brain hemorrhage. The other half are affected by, headaches, and stroke symptoms such as or hemiparesis.
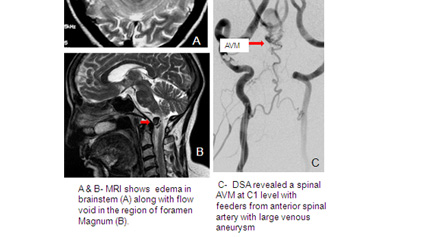
How is it diagnosed?
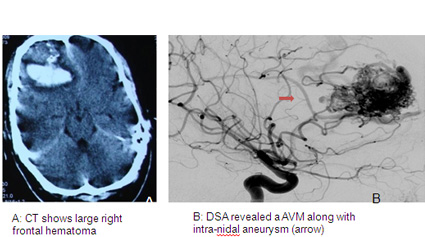
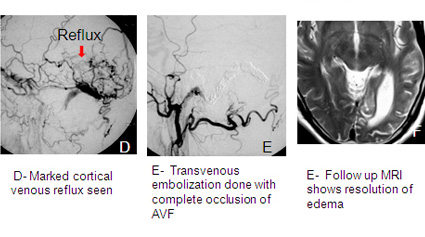
Often, the diagnosis of an AVM can be suspected by an expert radiologist with just CT scan of the brain. Most physicians, however, feel more comfortable diagnosing AVMs after performing an MRI. However AVMs can be missed on non-invasive imaging and for final diagnosis and evaluation by cerebral angiography is mandatory. In cases when bleeding has occurred, the AVM can be completely obscured by intracerebral bleeding, requiring a to establish a final diagnosis.
Why does it develop?
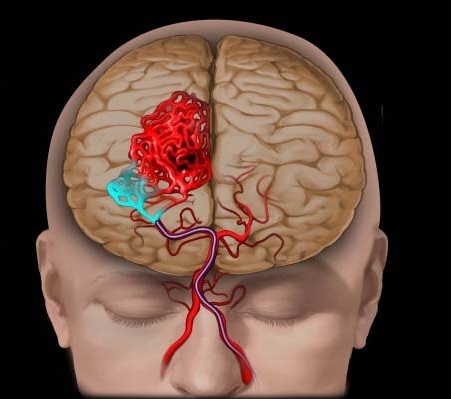
Brain AVMs affect about 0.1% of the population, and are present at birth, but they rarely affect more than one member of the same family. They happen roughly equally in men and women. AVMs are thought to be due to abnormal development of blood vessels in utero and may be present since birth. An AVM is not a cancer, and does not spread to other parts of the body. Dural AVFs, in adults are an acquired disorder that can occur probably after thrombosis of dural sinuses.
How is it treated?
There are 3 main modes of treatment. Endovascular embolization, micro neurosurgical excision and radiosurgery. These are given alone or in combination. Which of them is best for you is decided by our panel of experts after discussing your detailed clinical and radiological data. Your doctor will recommend the best treatment for you and this will be determined by the size of your AVM and also the location. It is not uncommon to recommend a combination of treatments.
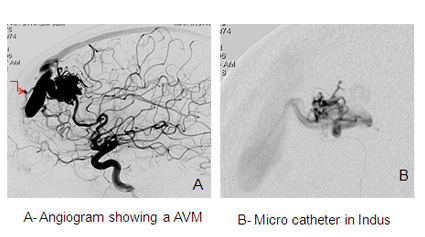
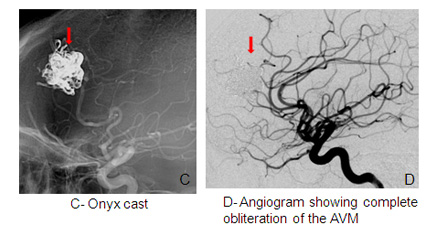
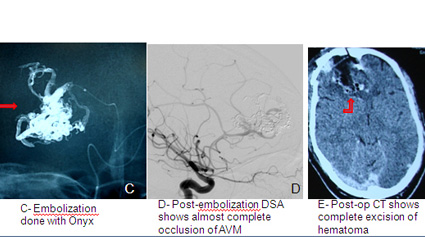
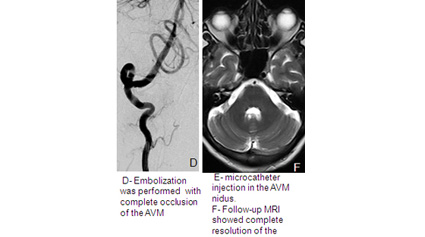
Embolization
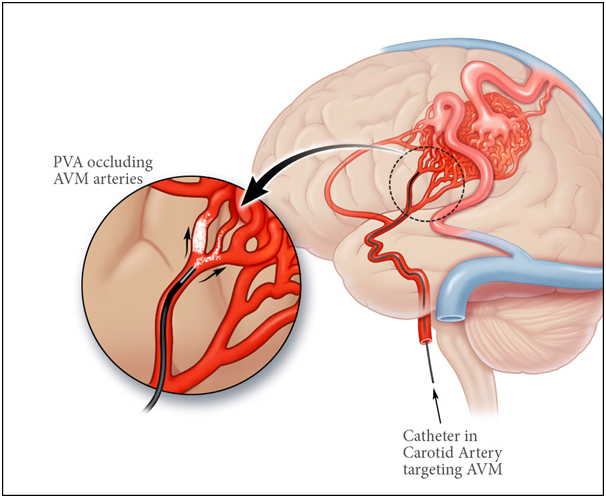
Under general anaesthesia a small catheter is advanced from the groin, into the brain vessels and then into the AVM. A liquid, non-reactive material (onyx) or glue is injected into the vessels which block the AVM off. There is a small risk to this procedure and the chances of completely curing the AVM using this technique depend on the size of the AVM. It is frequently combined with the other treatments such as radiation or surgery or it can be staged in multiple sessions .
Radiation Treatment
This treatment is also known as Radio surgery or Stereotactic Radiotherapy. A narrow x-ray beam is focused on the AVM such that a high dose is concentrated on the AVM with a much lower dose delivered to the rest of the brain. This radiation causes the AVM to shrivel up and close off over a period of 2-3 years in up to 80% of patients. The risk of complications is low. Until the AVM is completely closed off, the risk of bleeding still persists. This treatment can only be performed in small size AVM.
Surgery
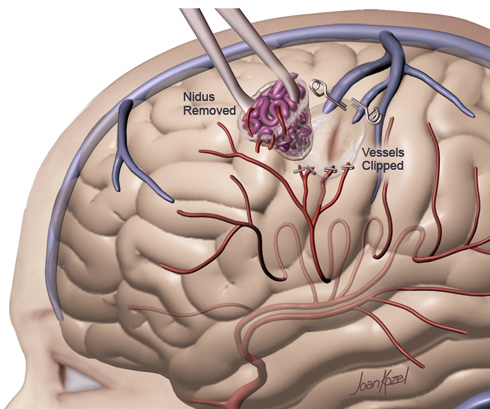
This is the oldest method for treating AVMs. The AVM is surgically removed in an operating room under general anesthesia. Since AVMs do not grow back, the cure is immediate and permanent if the AVM is removed completely. The risks of surgery are considered to be high for AVMs that are located in deep parts of the brain with very important functions. So surgery is usually indicated in those patient who are bled with large hematoma or the AVM is superficial and in non eloquent part of the brain.
Are there any alternatives?
Other than above mentioned modes of therapy no alternative is available. Only other option is to do nothing at all and just monitor the AVM. Your doctors may recommend observation if they feel that treatment can not be offered safely or when an AVM is discovered at a late age.
What will happen if it is left untreated?
There is risk of bleeding at the rate of 1-2 %/year after the diagnosis. But risk is much more if the AVm has bled or has a weak spot such as as aneurysm. Cumulative risk of bleeding is high depending upon the expected life expectancy.